Treating Parkinson's disease with AI: scientists propose an updated method
Kyiv • UNN
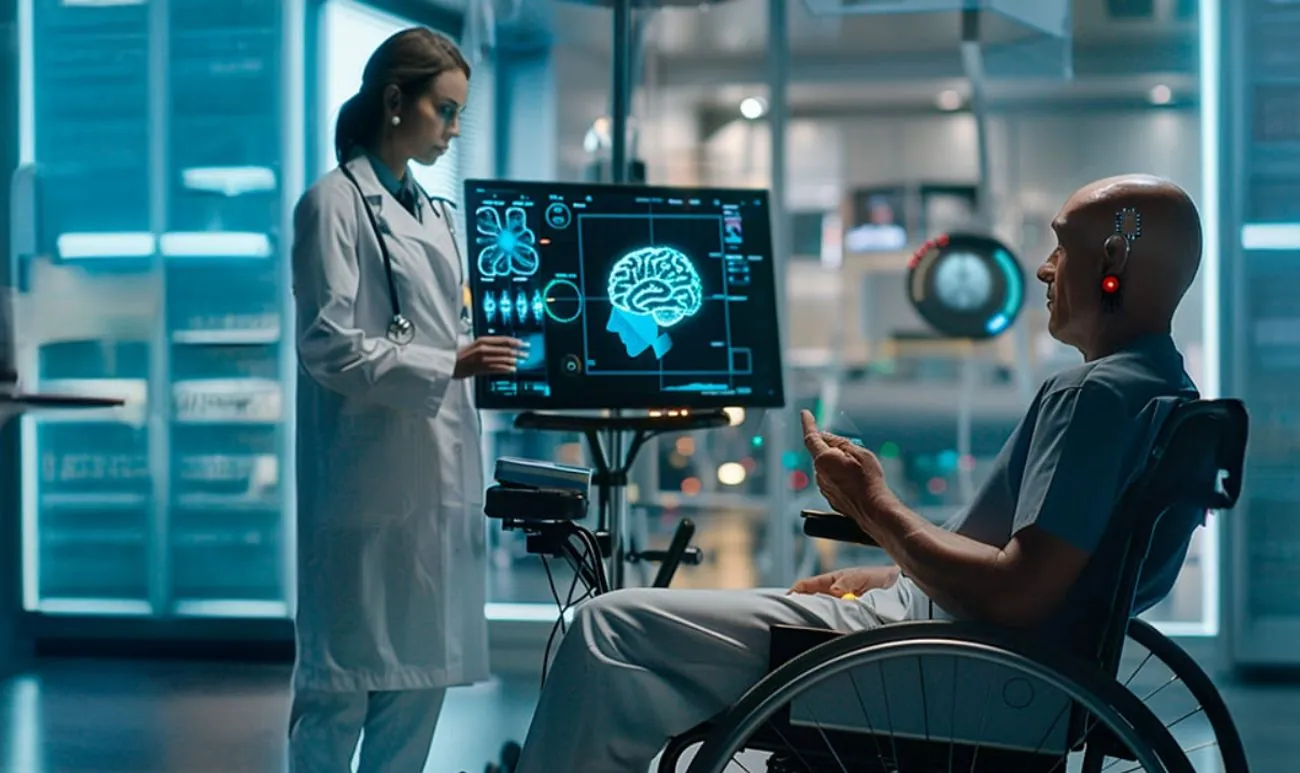
Adaptive deep brain stimulation using AI significantly reduced motor symptoms of Parkinson's disease. The new method personalizes therapy based on the patient's real-time brain activity.

Adaptive deep brain stimulation has virtually eliminated the most debilitating motor symptoms in some patients with Parkinson's disease. This has given scientists hope that the new method can help many other patients with the disease.
This is reported by UNN with reference to the Washington Post.
Features of Parkinson's disease
Like the heart, the brain has normal rhythms of electrical activity produced by neurons. Diseases such as epilepsy and schizophrenia are associated with abnormal brain rhythms, similar to cardiac arrhythmias. And in Parkinson's disease, neurons in the brain become too synchronized in a so-called oscillopathy. This can interfere with normal information transmission and lead to symptoms such as tremor and stiffness.
Imagine you're in a crowd, and there's a hum of conversation, but you can easily hear your own conversation — that's a normal situation of broadband neural activity. But with oscillopathy, it's like a protest march where everyone is chanting the same thing, and you can't hear yourself speak
Methods of combating the disease
Deep brain stimulation (DBS) is a surgical therapy for treating the symptoms of Parkinson's disease. A device similar to a pacemaker is implanted in the brain to deliver electrical impulses. This treatment method has been used since 1997.
Adaptive brain stimulation method
According to experts, DBS and Parkinson's disease medications weaken oscillopathy in the brain. In particular, constant electrical impulses from DBS help stimulate neuron activation in such a way, returning brain rhythms to normal.
Conventional DBS provides electrical stimulation at a constant setting. This can lead to periods of under- and overstimulation, which in turn leads to slowed movements or dyskinesia, respectively.
The updated, adaptive brain stimulation method personalizes therapy based on the patient's real-time brain activity using AI.
In February, the Food and Drug Administration approved the first adaptive DBS system for people with Parkinson's disease.
For some patients, especially those with more severe symptoms, standard DBS, which is always on in one constant mode, does not provide sufficient benefit. The brain's needs change depending on their activity level, for example, when they are awake or asleep, and especially according to the medication cycle
Hypotension: what it is and why it is dangerous21.10.24, 12:19 • 14910 views
Research
Previous studies have shown that adaptive DBS improves motor control, has fewer side effects, and delivers less electrical energy compared to conventional DBS.
In 2024, Starr and his colleagues conducted a pilot study involving four patients with Parkinson's disease. It found that adaptive DBS improved motor symptoms and quality of life compared to conventional DBS.
The researchers personalized the algorithms for each patient by bringing them to the clinic and measuring their brain rhythm while taking or excluding levodopa, a Parkinson's drug used to increase dopamine levels.
One way to develop these kinds of algorithms is to first do some brain signal studies under known conditions. Then you can train an artificial intelligence algorithm on this known data so that the AI program learns what combination of brain signals is associated with different states
Clinical trial
The ADAPT-PD clinical trial included 68 patients with Parkinson's disease who had previously been implanted with a conventional DBS system. They were fitted with adaptive DBS and sent home for 30 days.

Although the full results of the study have not yet been published, preliminary data showed no serious side effects, and 98% of participants chose to remain on adaptive DBS during long-term follow-up.
Risks and contraindications
Experts note that adaptive DBS or conventional DBS will not benefit every patient. Both motor and non-motor symptoms (postural instability, stiffness, gastrointestinal problems, and sleep problems) may still remain.
In addition, any surgery carries risks, and people with heart disease and high blood pressure are more likely to develop infection, stroke, brain hemorrhage, or anesthesia-related complications.
Not everyone with Parkinson's disease is a good candidate for any type of DBS. Patients must have a good response to dopaminergic drugs such as levodopa and should not be too advanced in their disease
Currently, scientists continue to improve adaptive deep brain stimulation, but hope that the new method can help many other patients with Parkinson's disease.